Rising PGY2 Seminar: Codes and RRT
Published in University of Utah Internal Medicine Residency Thursday Sem., 2024
Contributors: Alex Ryden, Sumit Patel, Ethan Krauspe, Mark Davis, Rodney Wayne, Brian Locke
License: Feel free to use and/or modify if attribution to original authors included.
Bookmark this if so inclined for future reference.
Agenda:
- Survey - link to RedCap
- 15-minute sessions on the needed microskills
- Leadership Style
- Rhythm Interpretation
- Do you have what you need?
- Identifying the Cause
- Ending the response
- Q&A and equipment
- Session Feedback link to RedCap
Pedagogical Note:
The right way to learn how to do this is:
- Watch someone run a code/RRT well
- Learn the key considerations*
- Imitate a well-run code/RRT (perhaps with simulation)
- Receive Feedback
Didactics are only 1 component of this.
Methods:
We’ve discussed with stakeholders and participants in the rapid response & code teams to identify the most common and consequential mistakes residents make:
- Unfavorable team dynamics emerge
- It’s not clear who is running the code.
- A shockable rhythm is not shocked.
- Decisions are too delayed.
- The person who activated the response gets snarked for a false alarm.
(please let us know of other events or near-misses)
The learning objectives:
- Discuss micro-skills/schemas to avoid each error.
We’re not going to review ACLS, per se:
Module 1: Leadership Style
Module 2: Pulse-Check Decisions
Module 3: Equipment and Personnel
Module 4: Identifying the Cause
Module 5: Ending the Code/RRT
Resources (Updated 5/16/2024)
| U of U | IMED | VA | |
|---|---|---|---|
| RRT/MET | House Sup, IM Res, SICU RN, Pharm | IM, STICU RN, Nurse Sup, Pharm, RT, EKG, ABG, Lab | IM, MICU, CNO, RNs, RT Pharmacy (7a-7p) |
| Code Blue | add: Anesth, EMT, MICU res, Pharm | add: ICU attgs | add: ED |
| Numbers | Shock Team, Cath, Brain Attack, VAD: 1-2222 | ‘Shock Team’: Vocera TICU attg, Brain Attack: Operator; x33333 | Brain attack: Page Neuro Senior, Cath: Page Cardiology, Code: x6 666 |
Coming soon: In-depth Code / RRT Guide
Q & A and Feedback
Post-session Survey: link to RedCap
Summary (TL;DR)
- Emphasize getting the right team dynamics
- “I’m Joe/Jane Doe, the resident on the code team. Who is running this code/RRT?” ”Can I take over?”
- Stand at the foot of the bed. Don’t move and don’t do tasks.
- Keep the big picture in mind:
- RRT: Is this a code? Does this patient need to go to the ICU?
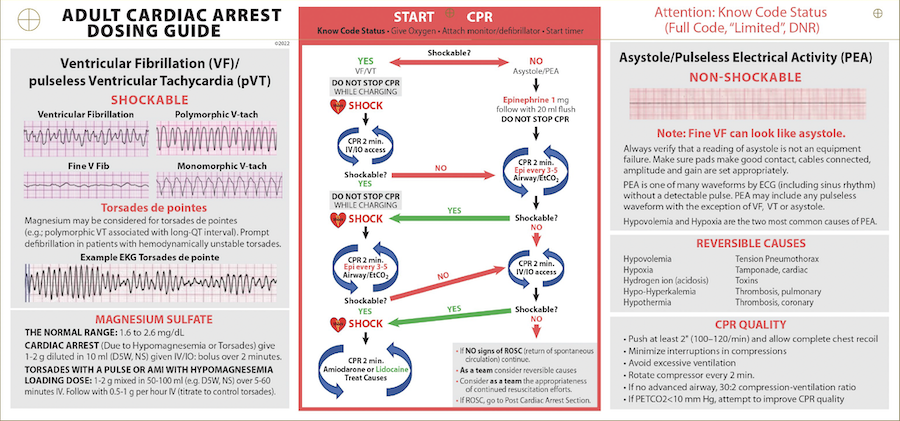
- Code: High quality compressions; shock if shockable
